Scott M. Weissman, Steve Bleyl, Alan Rope, Jacob E. Berchuck, Jamie Esposito, Colleen Caleshu, Katie Kobara
Implementation, utilization, and diagnostic outcomes
of a technology-enabled telehealth-based program for individuals to access multi-cancer early detection testing
Implementation, utilization, and diagnostic outcomes of a technology-enabled telehealth-based program for individuals to access multi-cancer early detection testing
Scott M. Weissman, Steve Bleyl, Alan Rope, Jacob E. Berchuck, Jamie Esposito, Colleen Caleshu, Katie Kobara
Background
Multi-cancer early detection (MCED) is a novel method to screen for many different cancers by detecting circulating tumor DNA in blood. Upon its commercial availability in 2021, we established two nation-wide telehealth programs that rely on digital tools to provide access to MCED in an efficient and scalable manner: 1) a patient-initiated program (PIP) and 2) an employer benefit program (EBP). Qualification for MCED was assessed via a digital tool for both programs, but the EBP required a consultation with a genetic counselor (GC) for individuals <50 years of age.
Aim
We investigated the implementation, utilization, and diagnostic outcomes of a technology-enabled telehealth program that provides access to MCED.
Methods
We performed a chart review of consecutive patients who presented for MCED from June 2021 – April 2022 in two separate programs – 1) an EBP for individuals aged 50 or older and those that were 18-49 years of age and had a GC consultation to determine eligibility based on personal and family history; 2) a PIP for individuals aged 40 or older through an automated questionnaire that assessed eligibility based on cancer risk factors. We extracted patient sex, age, risk criteria met, personal cancer history, test completion, and MCED results.
Results
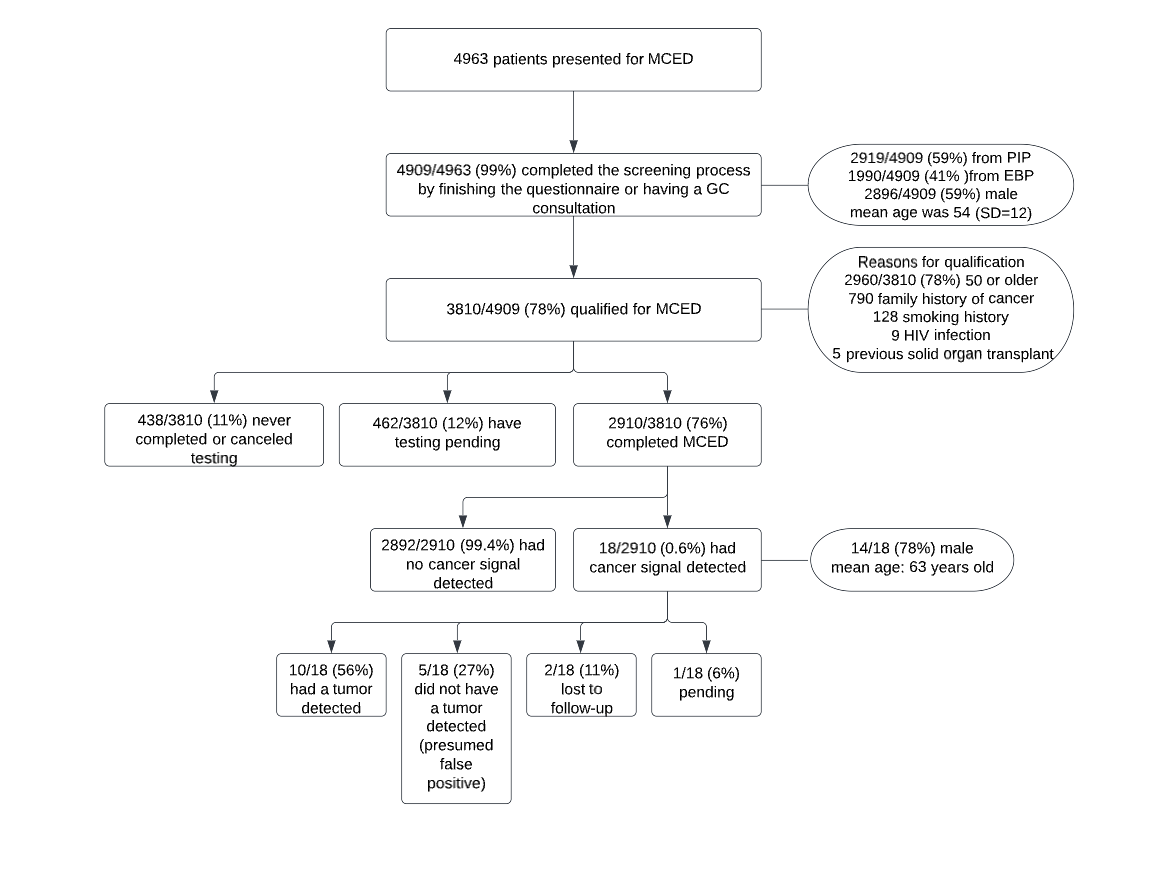
99% (4909/4963) of people completed the screening process by finishing the questionnaire or having a GC consultation. 59% (2919/4909) and 41% (1990/4909) came through the PIP and EBP, respectively. 59% were male (n=2896) and the mean age was 54 (SD=12). Overall, 78% (3810/4909) qualified for MCED. Of those, 78% (2960/3810) qualified based on age alone (50 or older). The remaining individuals (n=850) qualified because of a family history of cancer (790, 93%), smoking history (128, 15%), HIV infection (9, 1.1%), and/or previous solid organ transplant (5, 0.6%). Through the EBP, 23% (459/1990) of individuals met with a GC and of those, 55% (253/459) qualified for MCED. To date, 76% (n=2910) of individuals completed MCED, 12% (n=462) have testing pending, and 11% (n=438) never completed or canceled testing. 18 of the 2910 individuals with a completed test had a cancer signal detected (0.61%); mean age was 63 years (SD=8.7) and the majority were male (78%; 14/18). 50% (9) were diagnosed with cancer, 22% (4) were likely false positives, and 5 (28%) are still undergoing a clinical work-up.
Conclusion
MCED testing offered through a nation-wide telemedicine program had high utilization and completion of both the digital tool and testing. This suggests that a tech-enabled telehealth model can be used successfully to provide access to MCED with minimal barriers.
Background
Multi-cancer early detection (MCED) is a novel method to screen for many different cancers by detecting circulating tumor DNA in blood. Upon its commercial availability in 2021, we established two nation-wide telehealth programs that rely on digital tools to provide access to MCED in an efficient and scalable manner: 1) a patient-initiated program (PIP) and 2) an employer benefit program (EBP). Qualification for MCED was assessed via a digital tool for both programs, but the EBP required a consultation with a genetic counselor (GC) for individuals <50 years of age.
Aim
We investigated the implementation, utilization, and diagnostic outcomes of a technology-enabled telehealth program that provides access to MCED.
Methods
We performed a chart review of consecutive patients who presented for MCED from June 2021 – April 2022 in two separate programs – 1) an EBP for individuals aged 50 or older and those that were 18-49 years of age and had a GC consultation to determine eligibility based on personal and family history; 2) a PIP for individuals aged 40 or older through an automated questionnaire that assessed eligibility based on cancer risk factors. We extracted patient sex, age, risk criteria met, personal cancer history, test completion, and MCED results.
Results
99% (4909/4963) of people completed the screening process by finishing the questionnaire or having a GC consultation. 59% (2919/4909) and 41% (1990/4909) came through the PIP and EBP, respectively. 59% were male (n=2896) and the mean age was 54 (SD=12). Overall, 78% (3810/4909) qualified for MCED. Of those, 78% (2960/3810) qualified based on age alone (50 or older). The remaining individuals (n=850) qualified because of a family history of cancer (790, 93%), smoking history (128, 15%), HIV infection (9, 1.1%), and/or previous solid organ transplant (5, 0.6%). Through the EBP, 23% (459/1990) of individuals met with a GC and of those, 55% (253/459) qualified for MCED. To date, 76% (n=2910) of individuals completed MCED, 12% (n=462) have testing pending, and 11% (n=438) never completed or canceled testing. 18 of the 2910 individuals with a completed test had a cancer signal detected (0.61%); mean age was 63 years (SD=8.7) and the majority were male (78%; 14/18). 50% (9) were diagnosed with cancer, 22% (4) were likely false positives, and 5 (28%) are still undergoing a clinical work-up.
Conclusion
MCED testing offered through a nation-wide telemedicine program had high utilization and completion of both the digital tool and testing. This suggests that a tech-enabled telehealth model can be used successfully to provide access to MCED with minimal barriers.

